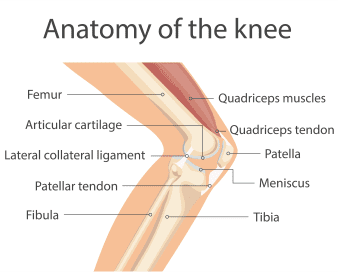
In the knee replacement procedure, each prosthesis is made up of four parts. The tibial component has two elements and replaces and the top of the shin bone or tibia. This prosthesis is made up of a metal tray attached directly to the bone and a high-density plastic spacer that provides the bearing surface. The femoral component replaces the bottom of the thigh bone or femur. This com¬ponent also replaces the groove where the patella or kneecap rides. The patellar component replaces the surface of the knee cap, which rubs against the femur. The patella protects the joint, and the resurfaced patellar button will slide smoothly on the front of the joint. In some cases, surgeons do not resurface the patella.
One of the keys to a successful implant is its ability to withstand the rigors of daily activity, and central to that is the quality of the artificial surfaces that slide against each other, or articulate, in the new joint. In knee implants, bearing surface options have been somewhat limited over the last few decades. The standard substance used for the femoral component is cobalt chrome, a metal alloy typified by its tough¬ness and biocompatibility. However, even this high-quality industry standard has its shortcomings. Over time, this metal surface can become roughened by bone and bone cement particles trapped between the femoral component and the plastic tibial insert.
This roughened surface, when rubbing against the plastic component up to two million times per year, can more quickly wear out your implant. When that happens, you will have to undergo surgery to replace the plastic piece, the femoral compo¬nent, and possibly even the tibial component. For this reason, implants have been shown to last between 10 and 15 years in the human body. The most exciting material to enter orthopaedics in recent years is OXINIUM° (oxi¬dized zirconium.)This remarkable new material combines the strengths of ceramic and metal, such as wear-reduction and strength, but does not have the weakness¬es, such as limited implant options and the possibility of fracture.
Zirconium is a biocompatible metal, similar to titanium. When the zirconium alloy undergoes a unique heating process, the surface of the metal transforms into a ceramic. Even though the new ceramic surface is 4,900 times more abrasion resistant than cobalt chrome, it retains the toughness and flexibility of the underlying metal. Because it can achieve this remarkable reduction in implant wear without sacri¬ficing strength as actual ceramic com¬ponents do, OXINIUM° implants have the potential to last significantly longer, thus possibly reducing the need for future corrective surgeries. When articulating on standard plastic tibial components, OXINIUM° knee implants reduce wear by 85-percent compared to cobalt chrome.
After your surgery is completed, you will be transported to the recovery room for close observation of your vital signs, circulation, and sensation in your legs and feet. As soon as you awaken and your condition is stabi¬lized, you will be transferred to your room. Below is an example of what you may see when you wake up:
- You will find a large dressing applied to your incision in order to maintain cleanliness and absorb any fluid.
- There may be a drain placed near your incision in order to record the amount of drainage being lost from the wound.
- You may be wearing elastic hose and/or a compression stocking sleeve designed to minimize the risks of blood clots.
- Your doctor may prescribe a PCA (patient-controlled analgesia) that is connect¬ed to your IV. The unit is set to deliver a small, controlled flow of pain medica¬tion and is enacted when you firmly press the button on your machine. Press the button anytime you are having pain.
- You may have a catheter inserted into your bladder as the side effects of anes¬thesia often make it difficult to urinate.